what is a pharmacy benefit manager
PBMs negotiate discounts from Wholesale Acquisition Cost WAC for quantity discounts that. A Pharmacy Benefit Manager is a critical component in the healthcare system especially in the United States.
 |
| Pharmacy Benefit Manager Comparison Of Drug Alternative Use Benmedica |
UnitedHealthcares pharmacy programs allow you to get the medication you need at a low cost.
. Ensures all customer service plan. According to the Pharmaceutical Care Management Association or PCMAT pharmacy benefit managers can help prevent up to one billion medication errors. Responsibilites of a PBM As the middleman PBMs handle many aspects of the entire process to ensure no drug misuse and overlook patient safety. A Pharmacy Benefit Managers Power of Negotiation.
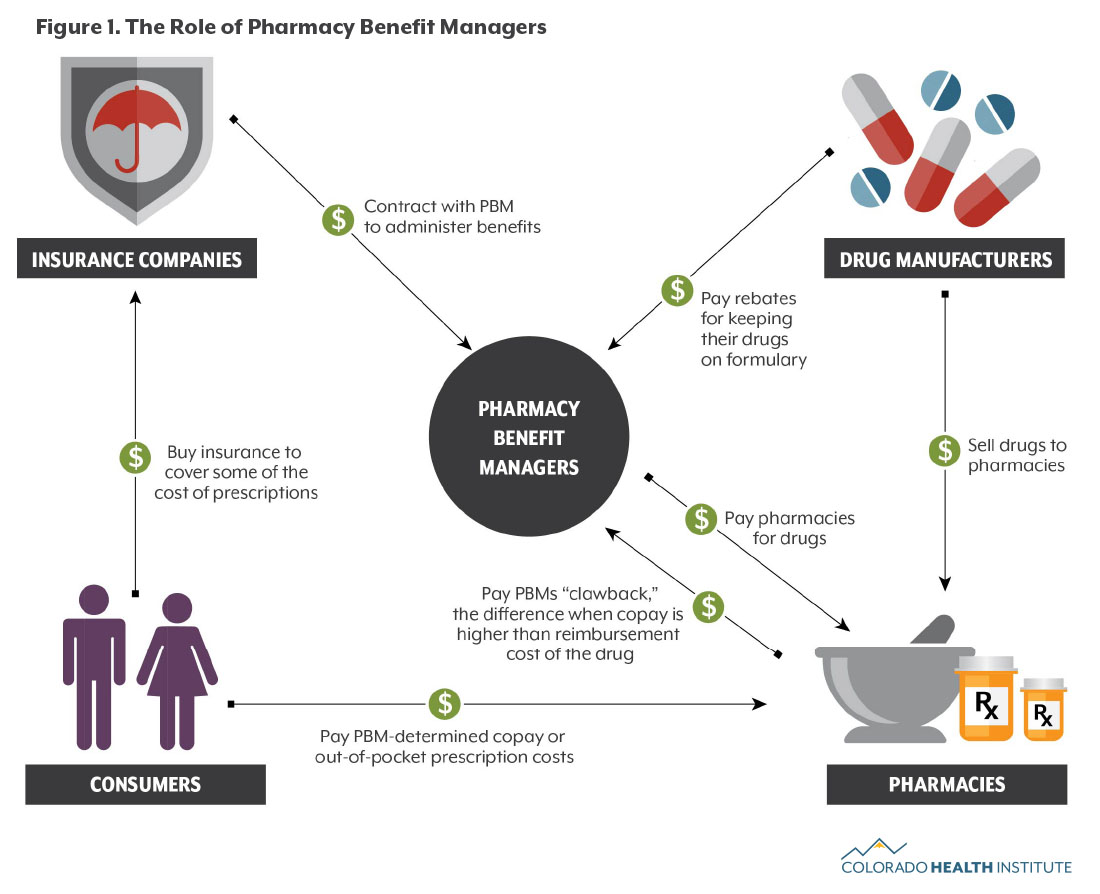
Pharmacy benefit managers connect employers insurance claimers drug wholesalers and pharmacies to provide service to people at the best possible costs. PBMs are contracted by employers to provide prescription drug benefit. Pharmacy Benefit Managers earn profits primarily through administrative fees charged for their services through spread pricing the difference between what is paid to. Pharmacy benefit managers PBMs are at the heart of the complicated supply chain that delivers prescription drugs from manufacturers to consumers.
A Pharmacy Benefit Manager or PBM is an intermediary between virtually every element of todays pharmacy benefits marketplace. A pharmacy benefits manager PBM is a third-party administrator TPA of prescription drug programs. In the United States a pharmacy benefit manager PBM is a third-party administrator of prescription drug programs for commercial health plans self-insured employer plans Medicare. Pharmacy benefits managers increase a patients access to medications by negotiating directly with drug manufacturers or wholesalers.
What is a Pharmacy Benefit Manager PBM. Their wide range of responsibilities. A pharmacy benefit manager is a corporation that manages prescription drug benefits on behalf of an insurance company. A PBM is a third-party administrator of a prescription drug program that is primarily responsible for processing and paying prescription.
A PBM processes prescription drug claims on behalf of plan sponsors such as employers government entities or unions. The system is complex and requires multiple stakeholders. Pharmacy benefit managers act as intermediaries between pharmaceutical corporations and health insurance providers. 4 minutes agoGlobal Pharmacy Benefit Management PBM Market 2022-2028 has been prepared based on an in-depth market analysis with inputs from industry experts.
While many people tend to assume that health. Express Scripts CVSCaremark and OptumRx are. From underwriters and reinsurers to pharmacy. Learn about our prescription benefits and health networks now.
What is a Pharmacy Benefit Manager PBM. Analysts expect full-year profit of. There are many different parties at play within the insurance industry. Manages the administrative and daily operationsprocedures of the relationship with the pharmacy benefit manager PBM.
Cigna now expects adjusted income from operations of at least 2310 per share compared with a prior forecast of at least 2290 per share.
 |
| Understanding Pbms Pharmacy Benefit Managers In Diabetes |
 |
| Pharmacy Benefit Manager Pbm Games Youtube |
 |
| Pharmacy Benefit Managers And Their Role In Drug Spending Commonwealth Fund |
 |
| Pbm Basics Pharmacists Society Of The State Of New York |
 |
| Pharmacy Benefit Management Pbm Market Size Industry Report 2026 |
Posting Komentar untuk "what is a pharmacy benefit manager"